Dr. Lindsay Broadbent shares her research studying the innate immune response to viral respiratory infections
Cytopathology and Immune Responses to Respiratory Viral Infections

Dr. Lindsay Broadbent is a postdoctoral fellow in the Wellcome-Wolfson Institute for Experimental Medicine at Queen’s University Belfast, where she studies the innate immune response to viral respiratory infections. In this Q&A, Lindsay shares how she and her colleagues are adapting their research to contribute to SARS-CoV-2 knowledge.
We will conduct a high-throughput screening of FDA-licensed drugs that could be repurposed for antiviral activity against SARS-CoV-2. Once we identify candidate drugs, we will use our differentiated primary respiratory epithelial cell model to optimize treatment dosage and efficacy.
Dr. Lindsay Broadbent
Please provide a general overview of your research interests.
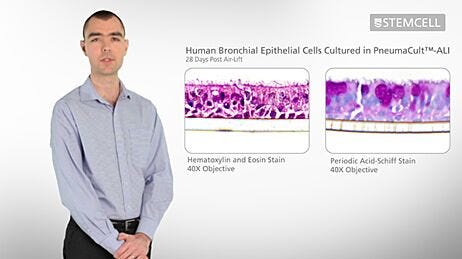
Human airway epithelial cells are one of the first lines of defense against pathogens invading the airways. To investigate the innate immune response to viral respiratory infections, we use differentiated airway epithelial cells. This authentically replicates the morphology of the in vivo human airways. These cultures are pseudostratified and consist of mucus-producing goblet cells, ciliated cells, and non-ciliated cells. We investigate cytopathology and innate immune responses to viral infections, primarily of the respiratory syncytial virus (RSV) and influenza.
Going back to when you first heard about this new coronavirus, what were some of your initial thoughts on how it would affect your research?
With our knowledge of respiratory viruses and our experience with primary airway epithelial cells, one of my first thoughts was, "How can we be of use?"
How are you (or your team) currently studying COVID-19?
Queen's University Belfast was one of the six UK research institutes to receive COVID-19 research funding from UK Research and Innovation (UKRI). I am collaborating with Professor Ultan Power and Professor Ken Mills, as well as other colleagues, to research possible COVID-19 therapeutic treatments. Initially, we will conduct a high-throughput screening of FDA-licensed drugs that could be repurposed for antiviral activity against SARS-CoV-2. Once we identify candidate drugs, we will use our differentiated primary respiratory epithelial cell model to optimize treatment dosage and efficacy. We will also monitor the innate immune response, which may be responsible for much of the damage associated with COVID-19.
What are some of the scientific challenges COVID-19 researchers are faced with?
Some of the challenges are listed below:
- SARS-CoV-2 is a containment level 3 (CL3) pathogen. To be able to work with this virus, the laboratory must be designed to work with dangerous viruses.
- For the safety of the researchers, appropriate personal protective equipment (PPE) must be worn and was initially difficult to source due to the pandemic.
- As this is a novel virus, there are not many reagents available for this specific pathogen. We spend a lot of time and effort to optimize protocols and products that were initially created for the first SARS virus research.
How are you using STEMCELL products in your research?
We use the PneumaCult™ medium to differentiate and maintain our primary respiratory epithelial cell cultures. The medium is used to culture bronchial epithelial cells from donors of different ages, sex, smoking status, and pre-existing conditions to screen for a COVID-19 treatment that works for a wide range of patients.
Related products: PneumaCult™-ALI-S Medium, PneumaCult™-ALI Medium, PneumaCult™-Ex Plus Medium, PneumaCult™-Ex Medium, PneumaCult™-ALI Medium
Explore These Resources
Request Pricing
Thank you for your interest in this product. Please provide us with your contact information and your local representative will contact you with a customized quote. Where appropriate, they can also assist you with a(n):
Estimated delivery time for your area
Product sample or exclusive offer
In-lab demonstration