Evaluating Hematopoietic Cell Therapy Product Potency Using the CFU Assay
Technical tip from our dedicated team of Product and Scientific Support specialists
There are unique challenges when it comes to cell therapy products, including ensuring the reproducibility and consistency of product lots. These specific concerns arise from the inherent variability of the starting material, which often comes from multiple patients or donors. Before using these cells as therapy, the quality–including both purity and potency–of the final product must be established. This in turn requires reliable cell assays.
The best type of assay to measure the functionality of hematopoietic stem and progenitor cells (HSPCs) is an in vivo mouse model engraftment study; however, these types of assays are time-consuming, expensive, and difficult to evaluate. Therefore, the in vitro colony-forming unit (CFU) assay, which has been shown to correlate well with in vivo engraftment models, is recommended to evaluate the quality of HSPCs used in cell therapy. Several cord blood bank accrediting bodies (including AABB and FACT) now require pre-freeze CFU data from cord blood collection, as evidence of sample stability and to ensure there is minimal loss of HSPCs during processing and cryopreservation.
In her webinar, Dr. Jackie Damen of STEMCELL Technologies explored the need for standardized potency assays for hematopoietic cell products and reviewed recent publications that evaluate the effects of cryopreservation protocols on the potency of cell therapy products. Dr. Damen defined the CFU assay and explored its utility as part of the cell therapy workflow. She also defined simple steps that can be taken to help ensure standardization of the CFU assay, including the use of automated imaging and analysis of cultures.
More recently, in his webinar, Dr. Colin Hammond from our Research and Development team discussed the regulatory guidance around the potency testing of hematopoietic, how to validate the CFU assay as a potency assay that can be integrated into cell therapy manufacturing workflows, and how to develop and validate a reference standard to help combat donor-to-donor variability.
In this article, Dr. Jackie Damen, Dr. Colin Hammond, and other experts from STEMCELL Technologies have answered some of the questions posed following the live webinars in April 2020 and June 2024. They have also supplied references for further reading.
Hematopoietic Stem and Progenitor Cell Biology
Where is the hematopoietic CD34+ stem cell niche?
Jackie Damen, PhD (Senior Scientific Advisor, Hematopoiesis): The hematopoietic CD34+ niche is found in the bone marrow. Niches are local tissue microenvironments that maintain and regulate stem cells. After birth, hematopoietic stem cells (HSCs) are found in a niche that starts in the long bone marrow cavities. Here, non-hematopoietic cells, including osteoblasts and marrow stromal cells, have been have been found to produce hematopoietic cytokines that support primitive haematopoiesis. For more information, refer to the review by Sean Morrison and David Scadden.
Further Reading
- Morrison SJ & Scadden DT. (2014) The bone marrow niche for haematopoietic stem cells. Nature 505(7483): 327–34.
Is the normal peripheral blood cell count range different in adolescents compared to adults?
Daniela Mora Ortiz, MD (Scientist, Scientific Support, Epithelial Cell Biology): Peripheral blood cell count differs slightly in the different age groups. At birth, the red blood cell (RBC) count is significantly higher compared to in early childhood and adults. The number declines within the first week of life since the lifespan of these erythroid cells is shorter. The counts fluctuate and stabilize at the end of the neonatal stage (birth - 28 days old).
The number of circulating CD34+ cells is higher closer to birth and then declines. At around 2 - 4 years old there is an abrupt change in HSC proliferative activity. This has been inferred from measurements of the rate of decline in telomere length of circulating leukocytes but overall, the hematopoietic system is modestly affected by aging until after the age of 65. The proliferative capacity of the marrow cells from older adults can sustain normal blood cell counts, but the reserve capacity may be limited, as observed by decreased responses to G-CSF with regards to mobilization of neutrophils and the response of CD34+ cells in older patients. In addition, marrow cellularity decreases with aging.
When blood is used as a source for stem cells, is there any additional testing for the potential presence of pathogens?
Dr. Jackie Damen: Yes, for cell therapy products used in gene therapies and more-than-minimally-manipulated cell therapies in prolonged cultures, regulations specify sterility testing for bacteria and fungi using microbial testing methods equivalent to or better than those described in 21 CFR 610.12. Federal regulations (21 CFR 1271: current Good Tissue Practices) require the collection, processing, packaging, and distribution of all cellular therapeutics by methods that prevent the introduction, transmission, or spread of communicable diseases, including viral, bacterial, fungal, and/or parasitic infections.
Further Reading
- Panch SR, et al. (2019) Prospective evaluation of a practical guideline for managing positive sterility test results in cell therapy products. Biol Blood Marrow Transplant 25(1): 172–78.
Can hematopoietic CD34+ cells be expanded ex vivo?
Dr. Jackie Damen: Investigation of the expansion of CD34+ cells ex vivo started in the 1990s and continues today. One breakthrough in the ex vivo culture of CD34+ cells was the discovery that bone marrow stromal cells and stromal cell lines in CD34+ culture could be replaced by serum-free media formulations, when combined with cytokines including SCF, Flt3,TPO, IL-3, and IL-6 in suspension cultures. Recently, high-throughput screening has identified new molecules; prostaglandin E2 (PGE), StemRegenin 1 (SR1), and UM171, that improve the frequency of the symmetric self-renewing HSC. Addition of these molecules results in higher numbers of the engraftable CD34+ cell compared to cultures with added cytokines alone.
Further Reading
- Tajer P et al. (2019) Ex vivo expansion of hematopoietic stem cells for therapeutic purposes: Lessons from development and the niche. Cells 8(2): 169.
Would you also recommend small molecules for the expansion of leukemic stem cells?
Leon Lin, PhD (Scientist, Research and Development): Yes, we recommend using UM729 for expansion of leukemic stem and progenitor cells. We have in-house data showing that UM729 at 1 μM performs similarly to UM171 at 175 nM in terms of maintenance and expansion of CD34+ and CD34+CD90+CD45RA- cells. The Sauvageau lab's original small molecule screen identified UM729 as capable of expanding acute myeloid leukemia (AML) leukemic stem and progenitor cells ex vivo (Pabst et al., 2014). Their more recent publication also utilized UM729 to culture AML cells to perform drug candidate screening (Baccelli et al., 2017).
Further Reading
- Pabst C et al. (2014) Identification of small molecules that support human leukemia stem cell activity ex vivo. Nat Methods 11(4): 436–42.
- Baccelli I et al. (2017) A novel approach for the identification of efficient combination therapies in primary human acute myeloid leukemia specimens. Blood Cancer J 7(2): e529.
How do you evaluate the lineage differentiation of the HSCs? For example, what defines an erythrocyte and is this identified through flow cytometry?
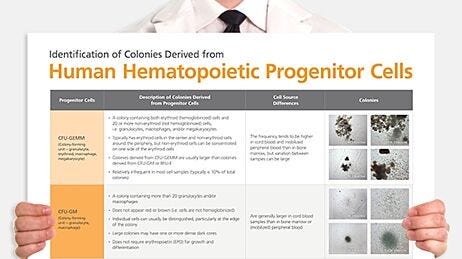
Once the progenitors grow and mature in an optimized formulation of MethoCult™ media, the result is colonies that contain mature cells that differ in size and color. Erythroid progenitors (BFU-E and CFU-E) will consist of small, red colored erythroblast cells at the edges of the colony and are distinctively different (when observed down the 10x objective of an inverted microscope) from myeloid colonies (CFU-GM), which consist of larger, clear and shiny granulocytes, monocytes, and macrophages.
The identity of mature cells within colonies from the various lineage types was confirmed historically using histological hematoxylin and eosin (H&E) staining as well as evaluation of lineage-specific surface marker expression using FACS.
For more, refer to the Atlas of Hematopoietic Colonies from Cord Blood.
How long can a mobilized blood sample be kept for transportation and maintain a viable and potent HSC population?
Dr. Jackie Damen: From publications reviewed in the webinar, the recommendation is to ensure mobilized PB and all samples of HSPC are stored at 4°C. The data from Janzen et al. (2009) showed cell viability and potency could be maintained for 48 hours, especially if the cell density is not excessively high (>50 million/mL). It is important to ensure that during shipping the cells do not come in contact with frozen ice packs. Depending on the downstream application, 24 hours post collection can be used as a cutoff to ensure good quality cells for additional processing steps.
Further Reading
- Jansen J et al. (2009) Transportation of peripheral blood progenitor cell products: Effects of time, temperature and cell concentration. Cytotherapy 11(1): 79–85.
How do iPSC-derived HSCs compare to bone marrow-derived (BM) HSCs and mobilized peripheral blood (mPB) HSCs in terms of the CFU assay?
Dr. Jackie Damen: The CD34+ cells derived from pluripotent stem cell (PSC) cultures are not functionally the same as the CD34+ cells derived from adult sources. Depending on the stage of embryogenesis from which the cells arise, their function at early stages of hematopoiesis are different. For example, lymphopoiesis is not required at primitive stages of development.
Depending on the method used to derive HSPCs from PSC cultures the total CFU frequency and lineage progenitor frequency can be very different. Most research has shown that the frequency of CFU/CD34 input is lower for PSC derived CD34+ cells (compared to both BM and mPB sources) and not all lineages are represented. In addition, the resulting colonies are typically smaller and tend to have fewer cells per colony since the progenitors do not seem to mature to the same extent as adult-derived CD34 cells in CFU cultures.
Can viruses used as vectors in cell and gene therapy cause infection?
Dr. Jackie Damen: Viruses used as vectors in cell and gene therapy are replication deficient and therefore cannot cause infection. Gene therapy approaches using viruses to infect hematopoietic stem cells as a treatment for hematological genetic disorders (like sickle cell disease and thalassemia) started in the early 1990s. Since then, various types of viral vectors have been evaluated and are replication deficient; however, their use in clinical trials using gene therapy have not been without risks resulting from immune responses, insertional mutagenesis, viral tropism, and off-target outcomes.
Further Reading
- Goswami R, et al. (2019) Gene therapy leaves a vicious cycle. Front Oncol 9: 297.
Applications of the CFU Assay in Cell Therapy
What would be the point of counting colonies in the CFU assay post engraftment?
Dr. Jackie Damen: The CFU assay provides retrospective information on the functional viability and potency of hematopoietic cell therapy products (HCTPs) as part of a QC test. Clinical labs may not count the specific numbers of colonies, instead reporting either ‘growth’ or ‘no growth’ as the result of the CFU assay. This would confirm that cells were still functionally viable at the time of injection, however it will not be known if patient engraftment has been successful until 2 - 4 weeks post transplant.
Processing labs, however, may define a specific plating concentration. In this case, the CFU growth or frequency that is reported indicates the minimum number of CFUs required for transplant, and is based on pre-freeze data. In addition, a review by Mike Watts, David Linch, and colleagues (2016) outlines results from a previous publication that shows neutrophil recovery within 14 days in >99% of patients (and none had a delayed engraftment beyond 28 days) when a CFU-GM dose of at least 2 x 10^5/kg was used so knowing this number can be informative. So, despite being retrospective, a minimum plating concentration of thawed cells in the CFU assay can confirm the dose and quality of the cells when neutrophil recovery in patients takes longer than 14 days.
Further Reading
- Watts MJ et al. (2016) Re-evaluation of progenitor thresholds and expectations for haematopoietic recovery based on an analysis of 810 autologous transplants: Implications for quality assurance. Br J Haematol 175(4): 673–76.
What is the difference between LTC-IC followed by CFU versus the CFU assay on its own? Which will be more accurate for comparison with an in vivo engraftment study?
Dr. Jackie Damen: The Long-Term Culture Initiating Cell (LTC-IC) assay uses the CFU assay as a readout but starts with co-culture of the earliest HSC on stromal cells, or stromal cell lines, without the additional requirement for cytokines. That said, present day protocols for this assay use a stromal cell line engineered to express critical human cytokines to make the assay more robust.
The LTC-IC assay enables measurement of the frequency of early HSCs in a test population following addition of this non-adherent cell population into cultures that have irradiated stromal cells. The protocol uses a limiting dilution strategy, requiring the initiation of replicate cultures (typically >12) of 4 - 6 cell dilutions of the test cell population. The cultures are then maintained for more than five weeks, with weekly half-media changes. At the end of the culture period all the non-adherent and adherent cells are harvested and plated into a CFU assay. Each replicate is plated into one CFU assay and after 14 days, the assays are evaluated as positive or negative for growth of progenitors. The frequency of negative replicates at each cell dilution can then be calculated and Poisson statistics used to determine the frequency of HSCs.
In theory, the LTC-IC assay would be expected to be more predictive of the in vivo engraftment assay. However it is a difficult assay and therefore not very robust—although there are publications from the 1990s that used this assay in lieu of the engraftment assay, which was developed later. Now, mostly because of improvements and the availability of new NSG mouse strains, the LTC-IC assay is not performed as much and does not appear in more recent publications in the field.
Learn more about the LTC-IC assay >Can you use the CFU assay for expanded or genetically modified CD34+ cells?
Colin Hammond, PhD (Scientist, Research and Development): The CFU assay can also be used to assess the ability of expanded or genetically modified HSPCs to form colonies. The efficiency of expanded or genetically modified cells to form colonies in the CFU assay will depend on the conditions of the expansion, including culture time and components of the culture medium, as well as the specifics of any editing procedure and genetic target. Ranges of plating densities should be used for these samples to ensure a scorable colony density is obtained.
Is it possible to characterize the subsets of the granulocytic lineage differentiated by CFU assay?
Dr. Jackie Damen: The granulocytic lineage consists of three mature cell types: neutrophils, basophils, and eosinophils. The only way to truly identify the frequency of these in peripheral blood is based on histological staining with hematoxylin and eosin (H&E) and evaluation of relevant morphological features that distinguishes these three types based on their size, color, and shape of the nucleus.
In a CFU assay, one only has the size of the mature cells to help identify the progenitor type and cannot visualize the shape of the nuclei. The shape of the nuclei is key in determining the difference between, for example, granulocytes and monocytes. The only way to identify the composition of the cells within a CFU-GM colony is to pluck the colony and evaluate the mature cells within the colony following a cytospin and subsequent H&E staining. However, most colonies are a heterogeneous mix of immature and mature cells that represents the lineage potential of the progenitor.
Alternatively, cells plucked from individual colonies can be stained with cell surface markers that are characteristic for the various mature cell types. However, this approach often involves staining of multiple surface markers to be definitive. Historically, histological staining, cell-surface expression by flow cytometry, and cytokine requirements have all been used to confirm lineage specific progenitor types.
Further Reading
- Görgens A et al. (2013) Revision of the human hematopoietic tree: Granulocyte subtypes derive from distinct hematopoietic lineages. Cell Rep 3(5): 1539–52.
Can the CFU assay be used for cells of the lymphoid lineage (T and B cells)?
Dr. Jackie Damen: Despite some early publications in the 1980's that suggested CFU cultures could be shown for T cells harvested from peripheral blood and the bone marrow, it was realized that growth and differentiation of lymphoid progenitors was limited to early pro-T and pro-B colonies only. The identification of Notch signaling as a crucial mediator for lymphopoiesis led to dramatically improved methods and expansion on the mouse bone marrow-derived stromal cell OP9 engineered to overexpress Notch ligand. This has greatly improved the ability to expand and derive mature human T cell subsets for therapeutic applications.
Further Reading
- Smith MJ et al. (2015) In vitro t-cell generation from adult, embryonic, and induced pluripotent stem cells: Many roads to one destination. Stem Cells 33(11): 3174–80.
Should I do the CFU assay when I obtain CD34+ cells, if my final objective is to obtain progenitor T cells after culture with the OP9-DL1 system?
Dr. Jackie Damen: If the objective is to obtain T cell progenitors, a CFU assay is only necessary to qualify the quality of the starting sample. Since the final product in this case is not expected to reconstitute the hematopoietic system in a compromised patient, the stability of frozen T cell products would not require the CFU assay. For T cell products, a different potency assay to identify T cell quality and function would be required. If, however, you are working on the production of engineered T cells to target and eliminate AML, then the CFU assay can be used to ensure there are no off-target effects of the T cells on CD34+ cells that could result in cytopenia.
Explore the StemSpan™ T Cell Generation Kit for differentiation of CD34+ cells to T Cells >
How correlative is the CFU assay to the engraftment efficiency of CD34+ cells in NSG mice?
Dr. Jackie Damen: There are a few examples of results from the CFU assays that correlate with good engraftment. Specifically, in a 2014 publication from Dr. Guy Sauvageau's lab (Fares et al, 2014), it was shown that when expanding cord blood CD34+ cells in the presence of UM171, there was an increase in the CD34+CD90+ population as well as in the numbers of the multipotential CFU-GEMM colonies. These two parameters correlated with an improvement in the frequency of HSCs, as determined by engraftment in the SCID repopulating cells (SRC) assay.
In addition, there seems to be good anecdotal data for this correlation: preliminary results presented in abstracts at meetings like ASH have shown trends in CFU frequency and colony size with engraftment potential and chimerism. Several translational studies have also concluded that the CFU-GM assay strongly correlates with successful patient recovery following a transplant.
We know also that when we expand CD34+ cells in culture, especially without the use of small molecules that support the self-renewing HSC divisions, and remove cells after 5 - 7 days to plate these in the CFU assay, two things are certain: the frequency of CFUs drop and colonies become smaller as their proliferative potential is exhausted. When there are no more progenitors that can be read out in the CFU assay, the expectation is that there would also be no cells capable of long term engraftment.
Further Reading
- Fares I et al. (2014) Pyrimidoindole derivatives are agonists of human hematopoietic stem cell self-renewal. Science (80) 345(6203): 1509–12.
For CFU assays evaluating CAR T cells, is it better to use CD34+ cord blood cells or bone marrow cells?
Dr. Colin Hammond: CAR-T hematotoxicity leading to bone marrow aplasia is a serious potential side effect of the treatment which can arise from off-target effects of the CAR-T cells on hematologically healthy cells. Therefore, the use of bone marrow cells or PBMCs may be more appropriate than cord blood cells in this context.
Since only 10 - 30% of CD34+ cells are typically measurable as CFU, does it mean the rest of cells are not early progenitors? Do the rest of the cells have very poor stemness that can not be measured, or does this mean that only about 30% of CD34+ cells maintain potency generally?
Dr. Colin Hammond: The cells that are measurable as CFU reflect a portion of the overall phenotypically defined (i.e. by CD34 positivity) HSPC compartment.
The conditions of the CFU assay support progenitors with erythroid and/or myeloid potential to be able to grow and form colonies. Under these conditions, typically 10 - 30% of the phenotypic CD34+ HSPC compartment are detected as erythroid and/or myeloid progenitors. Cells at different stages of the hierarchy, including early and later progenitors, can be measured as part of the CFU assay. Depending on their stage of maturity, progenitors exhibit different efficiencies of producing colonies, and more primitive progenitors can generally form larger colonies.
Due to the rarity of stem cells in the bulk CD34+ HSPC compartment, assays that more specifically probe their functionality, such as the LTC-IC assay or transplantation into immunodeficient mice, are required to determine their frequency. Similarly, progenitors with restricted lymphoid potential require alternate assays that are able to support their needs.
Cells that have very limited proliferative potential or die for one reason or another after plating also reduce the number of input cells that are ultimately detectable as CFU. Homeostatic maintenance of the blood system is generally highly polyclonal, but a reduction in the number of contributing clones has been reported as a potential feature of aging.
Does total CFU correlate with total CD34+ cells or viable CD34+ cell frequency?
Dr. Colin Hammond: CFU frequency is dependent on the frequency of viable functional progenitors in the sample. In fresh samples, this correlates quite well with the frequency of viable CD34+ cells. This correlation can drop in cases where the CD34+ cells are less functional than in a typical sample (e.g. from some ex vivo expansion strategies) or if the viability of the cells is overestimated (e.g. the effects of suboptimal cryopreservation on cell viability can take hours to days to manifest).
Further Reading
- Baust, J et al. (2009) Cryopreservation: An emerging paradigm change. Organogenesis 5(3):90-6
HSPC Sources and Reference Standards in the CFU Assay
What cell source is recommended for plating in the human CFU assay?
Dr. Colin Hammond: The choice of the sources of hematopoietic stem and progenitor cells (HSPCs) tested in the CFU assay is very dependent on the application. Hematopoietic cells are typically isolated from cord blood, bone marrow, or mobilized peripheral blood. Samples from these sources can be pre-enriched for HSPCs using CD34+ selection strategies or partially enriched to mononuclear cells (MNCs). Red blood cell lysis or removal at a minimum is highly recommended.
Additionally, reference standards should reflect the source of interest. For example, if testing the efficacy of gene editing workflows, mobilized peripheral blood CD34+ cells would be the recommended source of the reference standard since this is likely what will be required for the treatment of patients. Or, when evaluating the quality, potency, and stability of cord blood units, reference standards should be cord blood MNCs.
Automated scoring of colonies derived from healthy cord blood, bone marrow, and mobilized peripheral blood donors is validated for our STEMvision™ instrument. Other sources, such as diseased samples or PSC-derived HSPCs, will require specific validation in your workflow.
Learn more about the different sources of HSPCs here.
Do cells from cord blood and adults behave differently in the CFU assay?
Dr. Colin Hammond: Colonies arising from cord blood cells are typically larger than those from adult sources due to the increased proliferative activity of cord blood cells. This can impact the optimal number of cells to plate in a CFU assay to achieve reliably scorable cultures that are not overcrowded. The EU Pharmacopoeia sets a range of 40-80 colonies/CFU assay for cord blood cells. The ratio of BFU-E, CFU-GM, and CFU-GEMM can also vary between cord blood and adult sources.
Is there an expected ratio of CFU/BFU-E to CFU/GEMM that you expect from mobilized peripheral blood samples?
Dr. Colin Hammond: Mobilized peripheral blood (mPB), and especially non-mobilized peripheral blood, are highly variable in regards to the frequency of erythroid progenitors and therefore BFU-E. The resulting frequencies will also vary based on the mobilization strategy and efficiency of mobilization on the individual which can be very different based on health and age. The frequency of CFU-GEMM is typically quite low, cultures may contain none or a few depending on the total number of plated CFUs.
Can we use CFU samples from STEMCELL’s Proficiency Testing Program as a reference standard?
Dr. Colin Hammond: STEMCELL’s Proficiency Testing Program is designed to evaluate your ability to perform all the steps of the CFU assay, as well as upstream events such as cell thawing, dilution, inoculation, and plating. Participants are provided with a cell sample, MethoCult™ medium, additional reagents and supplies, and the detailed instructions required to perform the CFU assay. The results from all participants are analyzed and compared to the cohort mean according to guidelines outlined in ISO 13528. Samples provided as a part of the Proficiency Testing Program are not intended as a substitute for reference standards. Reference standards require in-house validation, for which human primary samples from STEMCELL including leukopaks, mononuclear cells, and CD34-enriched options can be used. STEMCELL’s Human Cord Blood Quality Control Kits are an option for routine verification of CFU workflow consistency in the lab which provide enough pretested cell aliquots to perform monthly testing for a year.
We currently don't use a control alongside our CFU assays, which from a regulatory point is a weakness, how could we best incorporate one?
Dr. Colin Hammond: Incorporation of a reference standard is the best way to test the accuracy of the CFU assay including all the critical parameters (such as equipment, reagents, and personnel) that affect the assay. A reference standard is a sample internally validated to have a known CFU output (i.e. the frequency of cells that can form a colony in the sample).
The source of HSPCs for reference standards should be the same as the test sample. These samples can be either purchased as large lots from a reliable vendor or from a patient/donor samples that have been deemed not appropriate for the desired application.
In most cases, multiple samples will ultimately be required to be validated for use as reference standards throughout the life of a project. Changes between different lots of reference standards will require bridging from one standard to another. At a minimum, reference standards should be evaluated on a regular basis including anytime there are changes to processes, staff, or equipment.
Do I have to include a new internal standard every time I run a test?
Dr. Colin Hammond: FDA Guidance for Industry regarding potency testing for product release specifies the use of “appropriate reference materials, standards, and/or controls”. The adequacy of your testing method and included controls or reference materials should be confirmed by the relevant regulatory agency. Reporting the relative potency of a test sample requires the comparison to a reference standard, necessitating the inclusion of a reference standard measurement whenever a test sample measurement is made during the workflow.
What if I run out of aliquots of my internal standard? Do I have to validate a new one?
Dr. Colin Hammond: Reference standards will eventually run out so it is important to validate a few samples that can be used and to keep renewing and validating new standards. As with all reference standards, it is important to also track each sample over time as functional attributes may deteriorate, though with proper long-term storage cryopreserved HSPCs can retain functionality for at least 10 years.
Monitoring of reference standard performance over time through the use of control charts can also alert to any anomalies that may indicate issues with reagents, equipment, or deviation from standard operating procedures.
Obtaining and validating several sufficiently large lots for use as reference standards early on will reduce the frequency that new lots will need to be validated.
Can the CFU assay be used for PSC-derived hematopoietic cells?
Dr. Colin Hammond: Yes, PSC-derived CD34+ cells can produce CFU colonies. It is worth noting that the CFU frequency is very dependent on the PSC line and how they were differentiated to hematopoietic cells, but is generally much lower than HSPCs isolated from normal healthy donors. We recommend using MethoCult™ SF H4636 or MethoCult™ SF H4636 Without EPO for performing CFU assays on human ESC or iPSC-derived cells.
CFU Assay Setup and Culture
Can the CFU assay be performed by sorting single cells into separate wells to ensure the final colony arises from that specific sorted cell?
Dr. Colin Hammond: CFU assays can be initiated from single sorted cells, and features of those cells at the time of sorting are correlated with their CFU activity. Validation, standardization, and correlation with clinical data to a level satisfactory to regulators would be required if incorporating this strategy into a cell and gene therapy workflow.
Further Reading
- Knapp, D, et al. (2019) A topological view of human CD34+ cell state trajectories from integrated single-cell output and proteomic data Blood 133(09):927-939.
Can a colony become resistant to MethoCult™ medium?
Dr. Colin Hammond: There is no evidence for this with regards to methylcellulose specifically (which is inert), but there are examples of hematological diseases that affect the sensitivity of progenitors to cytokines that are used in the media. For example, samples from some patients with Polycythemia Vera may produce erythroid colonies in the absence of erythropoietin.
- Scott, L, et al. (2006) Progenitors homozygous for the V617F mutation occur in most patients with polycythemia vera, but not essential thrombocythemia. Blood 108(7): 2435–2437.
What is the ideal MethoCult™ product for a CFU assay evaluating circulating CD34+ cells harvested from peripheral blood?
Dr. Colin Hammond: For CFU assays initiated from CD34-enriched samples, we recommend the MethoCult™ H4435 Enriched medium.
You can also use our CFU Assay Product Finder Tool to identify the recommended MethoCult™ medium for your application, as well as the consumables required to perform the CFU assay.
Can you share some tips on thawing HSPCs, specifically regarding the centrifuge speed?
Dr. Colin Hammond: Centrifugation at 300 x g is recommended. You can watch this video or read this step-by-step protocol to learn more about thawing frozen primary cells.
How can I keep my colonies separated in the CFU assay?
Dr. Colin Hammond: Colony distribution in the CFU assay should be mostly random if the cell suspension is well mixed with the MethoCult™ medium prior to plating. The presence of a meniscus in traditional 35 mm dishes means more MethoCult™ medium is present in the well, and therefore more of the cells embedded in the MethoCult™ will be at the edge of the well.
Use of meniscus-free SmartDish™ cultureware for the CFU assay aids in equally distributing the cells across the entire well area. However, colonies are highly variable in size and shape and can form very close to one another and even overlap with each other to varying degrees. This is less likely to occur at low plating densities (fewer colonies) than at higher plating densities (more colonies).
This is one of the reasons why plating test samples at multiple concentrations is important to achieve an optimal amount of colonies in each well, so that the amount of colony overlap is minimal and counting can be performed more reliably.
Is there a minimum number of colonies to consider satisfactory in the CFU assay?
Dr. Colin Hammond: The EU Pharmacopoeia specifies a range of 40 - 80 colonies/well for scoring cord blood CFU assays. Achieving these numbers is dependent on the robustness of the CFU assay performance in your lab, as well as the cell type, cell source, assay medium, and sample-specific performance.
For example, colonies produced by cord blood samples are typically larger than those from bone marrow or peripheral blood which can affect the range of accurately scorable colonies. Plating densities that yield too few colonies can cause higher variability in frequency and the ratio of colony types leading to potentially statistically inaccurate data.
Setting up multiple plating concentrations can provide information on assay accuracy for each test sample and help to yield an optimally scorable number of colonies.
How can we have the contents of the QC segment of the cord blood unit be more representative of the main bag?
Dr. Colin Hammond: The results obtained from attached QC segments have been reported to differ from the main bag due largely to the different sensitivity of the segment to environmental impacts such as transient thawing and ice crystal formation. Efforts to ensure adequate mixing of the main bag and segment components to distribute the cryoprotectant evenly, orienting segments on top of the main bag in the storage cassette, and reducing the impact of transient-warming events have shown some benefit to the representative performance of QC segments.
- Pasha R, et al. (2020) Transient warming affects potency of cryopreserved cord blood units. Cytotherapy 22(11): 690-697.
- Shoulars K, et al. (2015) Cord blood unit cryopreservation: Positioning segments for potency assessment. Blood 126(23): 4309.
- Kilbride P, et al. (2019) Recovery and post-thaw assessment of human umbilical cord blood cryopreserved as quality control segments and bulk samples. Transplantation and Cellular Therapy 25(12): 2447-2453.
Is trypan blue the most commonly used method for distinguishing live/dead, cells or would you recommend other stains? I noticed in your presentation that trypan staining-based cell counting can introduce errors from untrained personnel.
Dr. Jackie Damen: The use of trypan blue to evaluate cell viability has been used in cell culture for many years and can be performed manually (using a hemocytometer) or using automated cell counters. Viability determined manually with trypan blue is more subjective, based in part on the fact it is an exclusion dye compared to nuclear dyes like 7AAD that are more sensitive and robust. There is no consensus in the field to recommend a specific viability dye, but it is understood that trypan blue typically results in higher viability assessment when compared directly to 7AAD and AO/PI. Different viability stains can be used and validation with additional assays to confirm functional potency is typically required.
As far as a recommendation, I prefer using AO/PI staining. When we switched in the lab from using trypan blue to AO/PI, we realized that our viability for qualified lots of BM MNCs were in general ~10-15% lower but our CFU output was ~10 - 15% higher due to improved sensitivity of AO/PI compared to trypan blue.
Using trypan blue or 7ADD give us huge differences in the measured viability of thawed cord blood. Which method is more accurate to get the viability of the sample for plating into the CFU?
Dr. Colin Hammond: Dye and method differences for viability assessments and cell enumeration can have large impacts on the inferred number of viable cells in a given sample. For thawed samples, the time post-thaw at which viability is assessed can also lead to large variations in the number of viable cells counted, with earlier examination post-thaw typically having higher inferred viability than analysis at later time points. However, this may be misleading due to the fact that dye-based viability assessments usually correlate membrane integrity with cellular viability. Cells that have intact membranes immediately after thawing may go on to die later on due to stresses experienced during the freeze/thaw process. This means that early examination post-thaw may overestimate the actual viability of the cells in your thawed sample. Functional tests, such as the CFU assay, can prevent overestimation of viable functional cells, since the cells that die post-thaw, immediately or at later time points, will not go on to form colonies. Flow cytometry based viability assessments can also occasionally be misleading since there is a general difficulty in separating dead/dying cells from subcellular debris that can be captured in the same initial size and granularity gate. The viability assessment method ultimately used should be well documented and chosen for consistency and correlation with functional assays, such as the CFU assay.
Dr. Hammond mentioned in his webinar that it is good to plate a range of concentrations in the CFU assay to find that sweet spot for counting and determining morphology. Is this approach also helpful in getting a true count for the ratio of morphologies present, or that will always remain consistent across seeding concentrations?
Dr. Colin Hammond: The true frequency of colony lineage or classification should be consistent at each plating concentration—though it should be realized that the fewer the number of colonies observed, the more variability in colony types will be observed. In order to evaluate the ratio of morphologies present, multiple technical replicates should be evaluated. As an analogy, a low number of coin flips may indicate that the probability of landing on heads versus tails is different from the true 50:50 probability that is revealed from a larger number of flips.
With enough technical replicates, the ‘true’ frequency of each colony type can be determined even from low plating densities, but fewer replicates are required to determine this frequency if colony counts are higher but are still at non-saturating densities. For example, the more primitive CFU-GEMM colonies are fairly rare with generally zero to a few observable per well. The infrequency of CFU-GEMM colonies therefore requires many more technical replicates to be set up if aiming to determine their frequency in a given sample.
How many cells do you use to seed one plate when establishing viability using the CFU Assay?
Dr. Jackie Damen: The seeding density is dependent on the cell source and species when plating in the CFU Assay. For human samples, this is dependent on the frequency of CD34+ expected in these samples. Since this can vary between donors, we recommend ranges and plating 2 - 3 cell concentrations within the ranges (listed below) to ensure the CFU frequency is within the linear range and detection limits of the CFU assay.
Alternatively, if the percentage of CD34+ cells is known, the expectation is that there would be ~25% CFU per CD34+ cell plated (Serke, S. et al., 1991). So a more specific and appropriate plating concentration can be calculated from the number of CD34+ for each sample before plating.
Further Reading
- Serke S et al. (1991) Analysis of CD34-positive hematopoietic progenitor cells from normal human adult peripheral blood: Flow-cytometrical studies and in-vitro colony (CFU-GM, BFU-E) assays. Ann Hematol 62(2–3): 45–53.
- Watts MJ & Linch DC. (2016) Optimisation and quality control of cell processing for autologous stem cell transplantation. Br J Haematol 175(5): 771–83.
Can you please expand on recombinant cytokines regarding CFU Assays?
Dr. Jackie Damen: Optimal combinations and cytokine concentrations have been the subject of many investigations and attempts to standardize the CFU assay over the last 30 years. For human CFUs, most media formulations require appropriately qualified FBS with cytokine combinations that are optimal for the growth and differentiation of each progenitor type.
To visualize all the potential progenitors in a single patient sample for myelopoiesis, cytokine combinations that support the simultaneous growth of erythroid and myeloid progenitors have included recombinant human cytokines for SCF, GM-CSF, EPO, G-CSF, IL-3 and, in some cases, IL-6 if CD34+ are first purified.
Do you offer a ready-to-go cytokine mix as a supplement for the CFU assay?
Selena Hallahan, MSc (Product Manager, Hematology): We offer complete media for CFU assays, MethoCult™, which consists of methylcellulose media and supplements with prequalified serum, and cytokines optimized for human or mouse hematopoietic colony growth. For human cells our MethoCult™ H4034 Optimum is the best media for myeloid and erythroid colony growth from blood or bone marrow. We also offer serum-free formulations and cytokine-free versions, depending on what you need.
Use Our Interactive Product Finder to Find the Best Formulation for Your Experiment >
HSPC Colony Identification and Enumeration
How objective is the CFU assay? How does this affect the accuracy and reliability of the data?
Dr. Colin Hammond: The accuracy of the CFU assay relies on the standardization of critical parameters including methods, assay medium, equipment, and incubation conditions. Enumeration of colonies in the CFU assay can be somewhat subjective, particularly when carried out by manual operators. This can be reduced by comprehensive training and proficiency testing or by switching to automated methods to remove interpersonal bias. Testing should also be performed by different analysts to understand the robustness of the set up protocols and consistency of colony scoring in your workflow. Well-standardized workflows will exhibit more robust data quality and reproducibility.
How can CFU-GEMM colonies be used for statistical analysis since they are usually rare and low in numbers?
Dr. Colin Hammond: This is difficult due to the high donor-to-donor, colony growth and enumeration variabilities, and low frequency. An added complication can occur especially at higher densities where overlapping CFU-GM and BFU-E colonies may be misidentified as CFU-GEMM. Generally, for these, you would require many more technical replicates to obtain a reasonable number of these colonies to determine their frequency in the sample. For example, plating 10 - 30 replicate CFU assays may be needed to obtain sufficient numbers of CFU-GEMM for statistical analysis. Consultation with a biostatistician would also be recommended to ensure adequate power and sensitivity to evaluate your intended comparison.
Does STEMCELL offer CRO services? Can we use STEMCELL to validate data that we generate internally?
Dr. Colin Hammond: Yes, STEMCELL offers CRO services which can also be used to perform an independent assessment of samples. In addition, STEMCELL’s Contract Assay Services have previously provided CFU testing for novel drugs that have successfully gone onto IND submission. Enrollment in our global Proficiency Testing Programs is another strategy to evaluate your ability to perform all steps of the CFU assay.
Some colonies are reddish, but I can still see whitish cells under the higher power objective. Should it be considered BFU-E or CFU-GM?
Dr. Colin Hammond: In the differentiation of erythroid progenitors, the kinetics are such that these cells first need to exhaust their proliferative potential to induce maturation and hemoglobinization. In this process, the larger BFU-E are a mix of both mature and immature cells that are in the process of maturation. The immature erythroid cells can still appear “white” and are typically observed at the edge of the colony. These are distinct from CFU-GEMM which have larger, more obvious myeloid cells that have more spread from the colony whereas immature erythroid cells are typically smaller and in closer contact with the edges of BFU-E colonies.
Is the scoring of CFU assays subjective?
Dr. Jackie Damen: Yes, the scoring of CFU assays can be subjective. Some of the most common and particularly challenging phenomena encountered when scoring CFU colonies is the presence of colonies with multiple foci or clusters, which can be scored as separate colonies and thus erroneously skew the total counts to higher CFU numbers. This, in turn, may lead to an overestimation of HSPC graft potency. Conversely, high plating concentrations can result in overlapping and underdeveloped colonies that can lead to under-scoring of CFUs. Training has been shown to improve consistency between manual counters with regard to both identification of colony number as well as lineage identification of each colony type.
The regulations that we follow are from 1996, ISHAGE. Are there any actions by international societies when it comes to standardization of HCTPs?
Dr. Jackie Damen: There are other international societies, including the Joint Accreditation Committee ISCT-Europe (JACIE), which is an accreditation body for hematopoietic stem cell therapy. Their standards also require a potency assay for cell therapy products undergoing manipulation as well as for stability testing following storage. The CFU assay is suggested in addition to determination of CD34+ cell numbers; however, there is no mention of standardized protocols for these assays that I know of. Groups can validate their own assays and protocols and, with regards to those involving FACS, some publications have included the use of ALDH or the use of apoptotic dyes when evaluating viable CD34+ to ensure functional viability.
What is the procedure for standardizing CFU scoring without an automatic analyzer?
Dr. Colin Hammond: Rigorous staff training and proficiency testing can reduce variability in manual scoring. It is important to have staff practice with different donors and relevant sample types. Trained analysts should be performing CFU counts regularly to maintain aptitude over time and be refreshed in counting standards periodically. Inter-analyst variability in CFU scores can be determined by having multiple trained analysts score the same CFU assays.
STEMCELL Technologies offers on-demand and live virtual training in setting up, performing, and enumerating the hematopoietic progenitor CFU assay.
In addition, participants in STEMCELL’s CFU Assay Proficiency Testing Program can evaluate their ability to perform all the steps of the CFU assay, including enumeration, against a global cohort.
Why are the colony counts so different for each sample?
Dr. Colin Hammond: Colony counts in the CFU assay are a reflection of the functionality and frequency of viable progenitors in the original sample. The source of the sample (e.g. bone marrow or peripheral blood) and the age of the donor (e.g. cord blood, young adult, aged adult) can vary considerably in these aspects. Differential impacts of sample processing, storage, transportation, and culture conditions of the CFU assay (e.g. temperature, humidity, %CO2, time, etc) will also impact colony growth efficiency. Minimizing variation due to these technical aspects places the variation on the inherent donor-to-donor differences which can be accounted for by plating multiple cell densities in the CFU assay to capture a scorable colony density.
Automated CFU Scoring with STEMvision™
Why are the colony counts so different for each sample?
Dr. Colin Hammond: Colony counts in the CFU assay are a reflection of the functionality and frequency of viable progenitors in the original sample. The source of the sample (e.g. bone marrow or peripheral blood) and the age of the donor (e.g. cord blood, young adult, aged adult) can vary considerably in these aspects. Differential impacts of sample processing, storage, transportation, and culture conditions of the CFU assay (e.g. temperature, humidity, %CO2, time, etc) will also impact colony growth efficiency. Minimizing variation due to these technical aspects places the variation on the inherent donor-to-donor differences which can be accounted for by plating multiple cell densities in the CFU assay to capture a scorable colony density.
Can you give any examples on discrepancies between automated scoring and manual scoring?
Dr. Jackie Damen: When validating automated scoring, three errors can be identified: false positives (resulting from scratches or artifacts in the media and cultureware or overlapping colonies), false negatives (colonies not scored due to merging of colonies or colonies missed on the edges of the wells), and misidentified colonies (colonies that are scored as the wrong lineage).
Independent customer studies that have been shared with us have shown that correction of these errors, using the images available from colonies scored using STEMvision™ algorithms, resulted in data that was not statistically different. Differences in colony numbers and identification between corrected and uncorrected images were not significant. Similarly, the variability in counts from corrected and uncorrected images were shown to have similar or lower coefficients of variation (CVs) when using automated scoring compared to manual counting.
Find out more in the STEMvision™ Automated and Standardized Counting of CFU Assays for Cord Blood Banks Brochure.
How does STEMvision™ automated scoring compare to manual counting?
Dr. Jackie Damen: Validation studies to compare manual versus automated CFU counting have been investigated by various groups as part of their qualification process when switching from manual to automated CFU scoring. Internal studies carried out at STEMCELL show a strong correlation between manual and automated CFU scoring. These studies were carried out by comparing manual counts (performed by 3 to 7 experienced counters) of colony assays using cord blood, bone marrow, or mobilized peripheral blood, and comparing these counts to automated counts on a STEMvision™ instrument. Results showed an r value of 0.96 for total colonies, indicating a strong correlation between manual and automated CFU scoring.
Velier M et al. (2019) published that automated scoring using STEMvision™ reduces the coefficients of variation of repeatability, inter-operator variability, and intermediate precision.
Further Reading
- Velier M, et al. (2019) Validation of a semi automatic device to standardize quantification of colony-forming unit (CFU) on hematopoietic stem cell products. Cytotherapy 21(8): 820–23.
Is there a way to use STEMvision™ algorithms with bifocal microscope-acquired images?
Dr. Jackie Damen: Imaging with STEMvision™ is key to the way the STEMvision™ algorithm works and the algorithm cannot be used seperately to score images of colonies taken with a digital camera as the entire image is required for scoring with the STEMvision™ algorithms.
Is it possible to use custom scripts (e.g. ImageJ) to automate counting of the colonies?
Dr. Colin Hammond: STEMvision™ algorithms have been developed and validated to robustly count and identify colonies from normal healthy sources of hematopoietic cells in the CFU assay. You may be able to design custom analytical scripts that meet your specific needs. However, the large degree of heterogeneity of colony morphologies and donor/cell source specific variation presents a large challenge.
Is there capability for the report that STEMvision™ generates to include specifically CFU-GM/kg and/or CFU-GEMM/kg dose information?
Dr. Colin Hammond: Inputs from the user, including plating concentration, nucleated cell concentration and volume of the original sample, will yield calculations of total CFU per 10^5 nucleated cells, total CFU per mL of sample, and total CFU in the total unit. Extrapolation of these to evaluate sufficiency of a sample to meet dose requirements can proceed from the product CFU count over the recipient body weight (i.e. CFU dose = Product CFU count / Recipient weight).
Infusion TNC[x109] = (WBC/ mL + NRBC/mL [x106]) x infusion volume (mL)
TNC dose [x107kg] =
Post-thaw TNC recover [%] = x 100
Total CD34+ cells [x106] = CD34+ cells/ mL x dilution factor x 1000 mL x product volume(mL)
CD34+ cells [x105/kg] = Absolute CD34+ cell cells (x106 ÷ Recipient weight (kg)
Product RBC volume [mL] = product hematocrit x product volume (mL)
RBC dose [mL/kg] = Product RBC volume [mL] ÷ Recipient weight (kg)
Product CFU count [x105] =
CFU dose [x104/kg] = Product CFU count [x105 ÷ Recipient weight (kg)
Questions have been condensed and edited for clarity.
Explore These Resources
Request Pricing
Thank you for your interest in this product. Please provide us with your contact information and your local representative will contact you with a customized quote. Where appropriate, they can also assist you with a(n):
Estimated delivery time for your area
Product sample or exclusive offer
In-lab demonstration