Discerning the Link Between the Immune System and Endocrine Dysfunction

Dr. Dequina Nicholas is an Assistant Professor in the department of Molecular Biology and Biochemistry at the University of California, Irvine. Her research aims to understand how the immune system contributes to type 2 diabetes and polycystic ovarian syndrome (PCOS). In this interview, Dequina shares her scientific journey, her latest research, and her advice on how underrepresented groups in science can succeed in academia.
The Scientist: Dr. Dequina Nicholas
What inspired you to pursue a career in science?
This may sound super cheesy to say, but I wanted to pursue a career in science because I loved forensic science shows like Cold Case, CSI, and Bones. These TV shows made me think that science was the coolest thing ever. I had every intention of becoming a forensic scientist when I went to college, but once I was introduced to research, everything changed. Research contained everything that appealed to me about forensic science (problem solving, answering questions, solving mysteries, etc.), except I got to determine what questions were the most interesting!
Tell us about your scientific journey. How did you come to work in your current research field?
My first research experience was during undergrad as part of an honors program. I worked with a faculty member in the Chemistry Department to dehydrate alcohols using concentrated acids, and monitored the reaction by UV-Vis spectrometry. Although this project made me sure I did not want to be a chemist, I 100% loved the process and the challenge. I was given autonomy to run experiments on my own schedule and learned new analysis techniques from reading primary literature. Being a first-generation student, I had no clue that doing research could actually be a career. Long story short, a relative of a friend of my mom’s realized that I would be great in graduate school and convinced me to apply to a PhD program. In that program, my first rotation was in an immunology lab. Needless to say, I never looked back. The beautiful complexity of the immune system and how multiple molecules and cell types interact, and the powerful tool of flow cytometry hooked me. From then on, I was determined to be an immunologist and to work in a research area dear to my heart due to its prevalence in my family—type 2 diabetes. My mission since then has been to understand how the immune system contributes to metabolic disease and, ultimately, develop immunotherapies.
There will be plenty who will try to tell you that you are not good enough or don’t belong in science. That couldn’t be further from the truth. Pursuing a career in science can be very difficult, especially for underrepresented groups, but if you are following your passion, it is so fulfilling, and we can make it better for the next generation of students.
Dr. Dequina Nicholas
Lipid-Induced Immune Responses and Chronic Inflammation
Tell us about your latest research.
The lab is currently expanding into a topic that is new for us: the natural human immune response to lipid antigens. Lipid-induced immune responses are poorly understood and we are building new tools to evaluate lipid antigen-specific responses. We are also currently dissecting the contribution of immune cells in the pituitary to reproductive hormone secretion.
Inflammation is known to play a role in type 2 diabetes (T2D). In your 2019 Cell Metabolism publication, you found that T2D patients have high fatty acid availability, which ultimately promotes Th17 cytokine production in T cells, causing inflammation.1 Could you please elaborate on your findings, and do you find them surprising?
Yes, we initially began this project with the assumption and hypothesis that elevated glucose, which is the definition of T2D, is what is important for the T2D-related inflammation. We directly tested this in vitro and we observed that a lack of glucose had little effect on T2D-induced inflammation. Rather, blocking lipid metabolism ablated T2D-specific inflammation. Looking back, this is not too surprising of a finding knowing that Th17 cells, which dominate T2D inflammation, are dependent on lipid metabolism. Specifically, we found that in T2D, lipid metabolism is inefficient in immune cells, causing accumulation of lipid intermediates that, through an unknown mechanism, support Th17 inflammation. This mechanism is the subject of current projects in the lab.
As with type 2 diabetes, women with polycystic ovarian syndrome (PCOS) have elevated blood glucose, free fatty acids, and other nutrients. These nutrients are sensed by gonadotropes (endocrine cells in the anterior pituitary), which respond to these changes by adapting hormone production accordingly.2 In your 2020 Nature publication, you uncovered the mechanisms behind reproductive adaptations in response to nutrient availability, where you specifically reported on how gonadotropin-releasing hormone (GnRH) leads to increased glucose transporter 1 (GLUT1) protein expression in female gonadotropes, which in turn affects secretion of luteinizing hormone (LH). How do you think your findings could impact the field?
The field has known for a long time that reproduction is sensitive to nutrient availability, but the mechanisms have been unclear. This finding suggests cellular metabolism of the gonadotrope, which is downstream of other important regulators of reproduction, is a gatekeeping sensor of nutrient status, especially for females. This mechanism may be unifying for many of the reproductive phenotypes we see in disease states. For example, molecules that increase gonadotrope glycolysis likely increase luteinizing hormone, while we would expect the converse to be true. The role for GLUT1 in gonadotrope function provides a lens to understand how complex metabolic and systemic states, such as inflammation, obesity, fasting, and even fad diets impact the fertility of women. A clear understanding of how whole-body metabolism impacts gonadotrope cellular metabolism could translate into evidence-based dietary interventions for women with infertility issues.
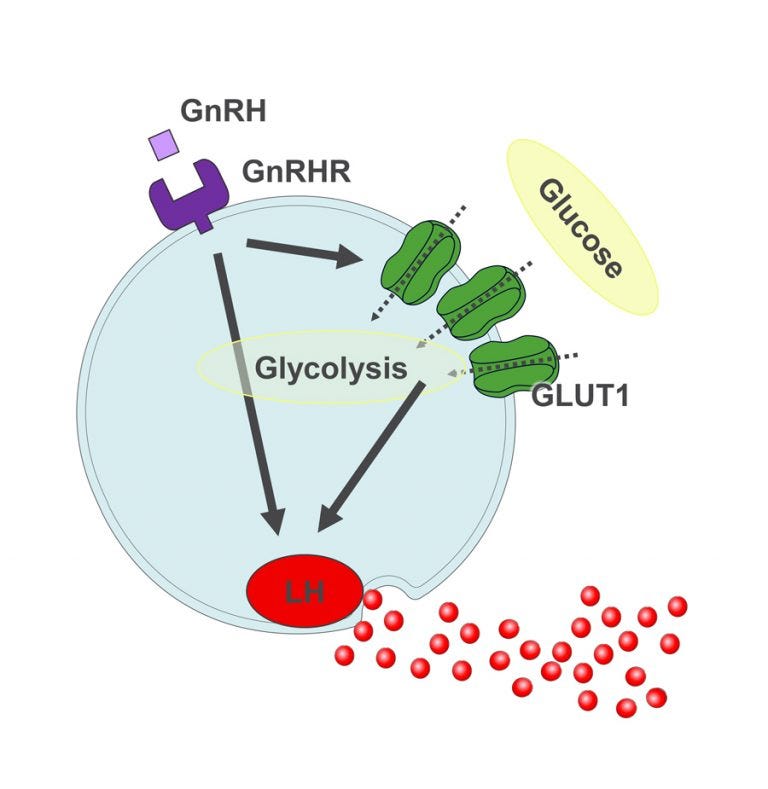
Figure 1. GLUT1-mediated glycolysis supports GnRH-induced secretion of luteinizing hormone in female gonadotropes.
*Image permission obtained by Dr. Dequina Nicholas.
Learn more about Dr. Nicholas’s research on gonadotropes in this video.
Where do you see your research going in the next 5 years?
Wow! That’s a loaded question. In terms of what our lab does, we are divided by two major research interests. One being type 2 diabetes and the other being PCOS. What ties these areas together is the common factor of chronic inflammation. We are hoping in the next 5 years to do the impossible: determine antigenic determinants of type 2 diabetes. We also hope to have a good grasp on the chronic inflammation associated with PCOS, with the goal of designing pre-clinical trials that target inflammation to improve disease.
Follow Dr. Nicholas on Twitter to stay updated on her journey and most recent research.
Advocating for Diversity and Mentorship in Science
What do you find most enjoyable and most challenging about research? Why?
The most enjoyable part of science is the journey with others. New pieces of data, creative approaches, troubleshooting, journal club—the amount of joy I get from these things is hard to put into words. Discovering something new that I know no one in the world has seen, or maybe hasn’t even thought about, is the best. I get so excited when my trainees share new data with me. Honestly, it’s a high and worth everything challenging about research. So, the most challenging part, at least to me, is that everything takes longer than you think. The delays are very difficult, especially because I am so invested in learning the answer to the questions we set out to answer. Delays can be experiments not working, reagents back-ordered, broken equipment, literally anything. Delays are beyond my control, so I just have to be patient and know that the data will come.
On your website you mentioned that you have received extensive training in teaching and mentoring diverse students in the classroom and laboratory. Do you have any advice for those from underrepresented groups who want to pursue a career in science?
YES! Please find mentors, find your people, find those who believe in you. There will be plenty who will try to tell you that you are not good enough or don’t belong in science. That couldn’t be further from the truth. Pursuing a career in science can be very difficult, especially for underrepresented groups. But if you are following your passion it is so fulfilling, and we can make it better for the next generation of students.
You recently published an article talking about establishing a laboratory or network during the pandemic and in the foreseeable future.3 What advice would you give to those who are looking to pursue that?
If I could only give three broad pieces of advice, it would be:
- Plan ahead way more than you are used to.
- If possible, find people at your new institution who have recently navigated setting up a lab and do not be shy in asking them EVERYTHING.
- Become best friends with your department’s administrative staff. You will need their help and you will enjoy their friendship.
Isolating Peripheral Blood Mononuclear Cells (PBMCs) and Lymphocytes
What cells do you isolate? Why do you need to isolate them for your research?
Our lab mainly separates PBMCs from whole blood samples. We use PBMCs and derivatives (CD4+ T cells, naïve T cells, B cells) to create cytokine profiles of people with and without disease and to test immune cell responses to newly identified antigens. We also use isolated immune cells for extracellular flux analysis since we are interested in the metabolism of these cells in different disease states.
Why did you decide to use SepMate™ to isolate your PBMCs, and how has it enabled you to advance your research?
We decided to use SepMate™ because sourcing cells was more reliable, and the specialized tubes really saved us a ton of time on the workflow. SepMate™ has allowed us to efficiently set up our biobank of human PBMCs and we continue to establish archives of new samples every week.
Before using SepMate™, what methods of isolation were you using?
To obtain cells from blood I have used an RBC lysis method in the past. We basically diluted the blood in an RBC lysis buffer then just pelleted the cells. This method is great if you want everything including platelets etc. With density gradient separation, we get clean PBMCs.
To obtain PMBCs, before SepMate™, we did density gradient separation using Ficoll-1077. Our protocol was essentially the same until we began using SepMate™ tubes. Carefully layering blood on top of density media, centrifuging with the brake off, and then carefully removing the buffy coat to get PBMCs was a very time-intensive task. We process 2 to 3 samples a week, so the wasted time was really adding up.
Learn More About Isolating Cells from Blood
Hassle-Free PBMC Isolation with SepMate™
Simplify your density gradient centrifugation and isolate your PBMCs in as little as 15 minutes using SepMate™.
Efficient Blood Sample Processing
Explore tips and tools for red blood cell depletion and cell isolation from blood samples.
View more Immunology Profiles or nominate yourself to be featured in your own profile.
References
- Nicholas D et al. (2019) Fatty Acid Metabolites Combine with Reduced β Oxidation to Activate Th17 Inflammation in Human Type 2 Diabetes. Cell Metab 30(3): 447–61.
- Nicholas D et al. (2020) GLUT1-mediated glycolysis supports GnRH-induced secretion of luteinizing hormone from female gonadotropes. Sci Rep 10(1): 1–19.
- Nicholas D, Trejo J & Termini C. (2022) Building a laboratory and networks during the COVID-19 pandemic. Trends Biochem Sci 47(9): 725–7.
Products to Isolate Immune Cells from Blood
Related Resources
Request Pricing
Thank you for your interest in this product. Please provide us with your contact information and your local representative will contact you with a customized quote. Where appropriate, they can also assist you with a(n):
Estimated delivery time for your area
Product sample or exclusive offer
In-lab demonstration