Evaluating Hematopoietic Cell Therapy Product Potency Using the CFU Assay
Technical tip from our dedicated team of Product and Scientific Support specialists
There are unique challenges when it comes to cell therapy products, including ensuring the reproducibility and consistency of product lots. These specific concerns arise from the inherent variability of the starting material, which often comes from multiple patients or donors. Before using these cells as therapy, the quality–including both purity and potency–of the final product must be established. This in turn requires reliable cell assays.
The best type of assay to measure the functionality of hematopoietic stem and progenitor cells (HSPCs) is an in vivo mouse model engraftment study; however, these types of assays are time-consuming, expensive, and difficult to evaluate. Therefore, the in vitro colony-forming unit (CFU) assay, which has been shown to correlate well with in vivo engraftment models, is recommended to evaluate the quality of HSPCs used in cell therapy. Several cord blood bank accrediting bodies (including AABB and FACT) now require pre-freeze CFU data from cord blood collection, as evidence of sample stability and to ensure there is minimal loss of HSPCs during processing and cryopreservation.
In her recent webinar, Dr. Jackie Damen of STEMCELL Technologies explored the need for standardized potency assays for hematopoietic cell products and reviewed recent publications that evaluate the effects of cryopreservation protocols on the potency of cell therapy products. Dr. Damen defined the CFU assay and explored its utility as part of the cell therapy workflow. She also defined simple steps that can be taken to help ensure standardization of the CFU assay, including the use of automated imaging and analysis of cultures.
In this article, Dr. Jackie Damen and her colleagues from STEMCELL Technologies have answered some of the questions that were posed following the live webinar in April 2020. They have also supplied references for further reading.
Hematopoietic Stem and Progenitor Cell Biology
Where is the hematopoietic CD34+ stem cell niche?
Further Reading
- Morrison SJ & Scadden DT. (2014) The bone marrow niche for haematopoietic stem cells. Nature 505(7483): 327–34.
Is the normal peripheral blood cell count range different in adolescents compared to adults?
Daniela Mora Ortiz, MD (Scientific Operations Associate & Lab Manager): Peripheral blood cell count differs slightly in the different age groups. At birth, the red blood cell (RBC) count is significantly higher compared to in early childhood and adults. The number declines within the first week of life since the lifespan of these erythroid cells is shorter. The counts fluctuate and stabilize at the end of the neonatal stage (birth - 28 days old).
The number of circulating CD34+ cells is higher closer to birth and then declines. At around 2 - 4 years old there is an abrupt change in HSC proliferative activity. This has been inferred from measurements of the rate of decline in telomere length of circulating leukocytes but overall, the hematopoietic system is modestly affected by aging until after the age of 65. The proliferative capacity of the marrow cells from older adults can sustain normal blood cell counts, but the reserve capacity may be limited, as observed by decreased responses to G-CSF with regards to mobilization of neutrophils and the response of CD34+ cells in older patients. In addition, marrow cellularity decreases with aging.
When blood is used as a source for stem cells, is there any additional testing for the potential presence of pathogens?
Further Reading
- Panch SR, et al. (2019) Prospective evaluation of a practical guideline for managing positive sterility test results in cell therapy products. Biol Blood Marrow Transplant 25(1): 172–78.
Can hematopoietic CD34+ cells be expanded ex vivo?
Further Reading
- Tajer P et al. (2019) Ex vivo expansion of hematopoietic stem cells for therapeutic purposes: Lessons from development and the niche. Cells 8(2): 169.
Would you also recommend small molecules for the expansion of leukemic stem cells?
Further Reading
- Pabst C et al. (2014) Identification of small molecules that support human leukemia stem cell activity ex vivo. Nat Methods 11(4): 436–42.
- Baccelli I et al. (2017) A novel approach for the identification of efficient combination therapies in primary human acute myeloid leukemia specimens. Blood Cancer J 7(2): e529.
How do you evaluate the lineage differentiation of the HSCs? For example, what defines an erythrocyte and is this identified through flow cytometry?
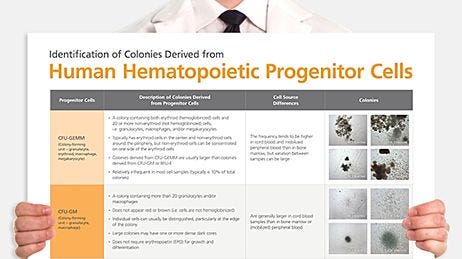
Once the progenitors grow and mature in an optimized formulation of MethoCult™ media, the result is colonies that contain mature cells that differ in size and color. Erythroid progenitors (BFU-E and CFU-E) will consist of small, red colored erythroblast cells at the edges of the colony and are distinctively different (when observed down the 10x objective of an inverted microscope) from myeloid colonies (CFU-GM), which consist of larger, clear and shiny granulocytes, monocytes, and macrophages.
The identity of mature cells within colonies from the various lineage types was confirmed historically using histological hematoxylin and eosin (H&E) staining as well as evaluation of lineage-specific surface marker expression using FACS.
For more, refer to the Atlas of Hematopoietic Colonies from Cord Blood.
How long can a mobilized blood sample be kept for transportation and maintain a viable and potent HSC population?
Further Reading
- Jansen J et al. (2009) Transportation of peripheral blood progenitor cell products: Effects of time, temperature and cell concentration. Cytotherapy 11(1): 79–85.
How do iPSC-derived HSCs compare to bone marrow-derived (BM) HSCs and mobilized peripheral blood (mPB) HSCs in terms of the CFU assay?
Dr. Jackie Damen: The CD34+ cells derived from pluripotent stem cell (PSC) cultures are not functionally the same as the CD34+ cells derived from adult sources. Depending on the stage of embryogenesis from which the cells arise, their function at early stages of hematopoiesis are different. For example, lymphopoiesis is not required at primitive stages of development.
Depending on the method used to derive HSPCs from PSC cultures the total CFU frequency and lineage progenitor frequency can be very different. Most research has shown that the frequency of CFU/CD34 input is lower for PSC derived CD34+ cells (compared to both BM and mPB sources) and not all lineages are represented. In addition, the resulting colonies are typically smaller and tend to have fewer cells per colony since the progenitors do not seem to mature to the same extent as adult-derived CD34 cells in CFU cultures.
Can viruses used as vectors in cell and gene therapy cause infection?
Further Reading
- Goswami R, et al. (2019) Gene therapy leaves a vicious cycle. Front Oncol 9: 297.
Applications of the CFU Assay in Cell Therapy
What would be the point of counting colonies in the CFU assay post engraftment?
Dr. Jackie Damen: The CFU assay provides retrospective information on the functional viability and potency of hematopoietic cell therapy products (HCTPs) as part of a QC test. Clinical labs may not count the specific numbers of colonies, instead reporting either ‘growth’ or ‘no growth’ as the result of the CFU assay. This would confirm that cells were still functionally viable at the time of injection, however it will not be known if patient engraftment has been successful until 2 - 4 weeks post transplant.
Processing labs, however, may define a specific plating concentration. In this case, the CFU growth or frequency that is reported indicates the minimum number of CFUs required for transplant, and is based on pre-freeze data. In addition, a review by Mike Watts, David Linch, and colleagues (2016) outlines results from a previous publication that shows neutrophil recovery within 14 days in >99% of patients (and none had a delayed engraftment beyond 28 days) when a CFU-GM dose of at least 2 x 10^5/kg was used so knowing this number can be informative. So, despite being retrospective, a minimum plating concentration of thawed cells in the CFU assay can confirm the dose and quality of the cells when neutrophil recovery in patients takes longer than 14 days.
Further Reading
- Watts MJ et al. (2016) Re-evaluation of progenitor thresholds and expectations for haematopoietic recovery based on an analysis of 810 autologous transplants: Implications for quality assurance. Br J Haematol 175(4): 673–76.
What is the difference between LTC-IC followed by CFU versus the CFU assay on its own? Which will be more accurate for comparison with an in vivo engraftment study?
Dr. Jackie Damen: The Long-Term Culture Initiating Cell (LTC-IC) assay uses the CFU assay as a readout but starts with co-culture of the earliest HSC on stromal cells, or stromal cell lines, without the additional requirement for cytokines. That said, present day protocols for this assay use a stromal cell line engineered to express critical human cytokines to make the assay more robust.
The LTC-IC assay enables measurement of the frequency of early HSCs in a test population following addition of this non-adherent cell population into cultures that have irradiated stromal cells. The protocol uses a limiting dilution strategy, requiring the initiation of replicate cultures (typically >12) of 4 - 6 cell dilutions of the test cell population. The cultures are then maintained for more than five weeks, with weekly half-media changes. At the end of the culture period all the non-adherent and adherent cells are harvested and plated into a CFU assay. Each replicate is plated into one CFU assay and after 14 days, the assays are evaluated as positive or negative for growth of progenitors. The frequency of negative replicates at each cell dilution can then be calculated and Poisson statistics used to determine the frequency of HSCs.
In theory, the LTC-IC assay would be expected to be more predictive of the in vivo engraftment assay. However it is a difficult assay and therefore not very robust—although there are publications from the 1990s that used this assay in lieu of the engraftment assay, which was developed later. Now, mostly because of improvements and the availability of new NSG mouse strains, the LTC-IC assay is not performed as much and does not appear in more recent publications in the field.
Learn more about the LTC-IC assay >Is it possible to characterize the subsets of the granulocytic lineage differentiated by CFU assay?
In a CFU assay, one only has the size of the mature cells to help identify the progenitor type and cannot visualize the shape of the nuclei. The shape of the nuclei is key in determining the difference between, for example, granulocytes and monocytes. The only way to identify the composition of the cells within a CFU-GM colony is to pluck the colony and evaluate the mature cells within the colony following a cytospin and subsequent H&E staining. However, most colonies are a heterogeneous mix of immature and mature cells that represents the lineage potential of the progenitor.
Alternatively, cells plucked from individual colonies can be stained with cell surface markers that are characteristic for the various mature cell types. However, this approach often involves staining of multiple surface markers to be definitive. Historically, histological staining, cell-surface expression by flow cytometry, and cytokine requirements have all been used to confirm lineage specific progenitor types.
Further Reading
- Görgens A et al. (2013) Revision of the human hematopoietic tree: Granulocyte subtypes derive from distinct hematopoietic lineages. Cell Rep 3(5): 1539–52.
Can the CFU assay be used for cells of the lymphoid lineage (T and B cells)?
Further Reading
- Smith MJ et al. (2015) In vitro t-cell generation from adult, embryonic, and induced pluripotent stem cells: Many roads to one destination. Stem Cells 33(11): 3174–80.
Should I do the CFU assay when I obtain CD34+ cells, if my final objective is to obtain progenitor T cells after culture with the OP9-DL1 system?
Dr. Jackie Damen:If the objective is to obtain T cell progenitors, a CFU assay is only necessary to qualify the quality of the starting sample. Since the final product in this case is not expected to reconstitute the hematopoietic system in a compromised patient, the stability of frozen T cell products would not require the CFU assay. For T cell products, a different potency assay to identify T cell quality and function would be required. If, however, you are working on the production of engineered T cells to target and eliminate AML, then the CFU assay can be used to ensure there are no off-target effects of the T cells on CD34+ cells that could result in cytopenia.
Explore the StemSpan™ T Cell Generation Kit for differentiation of CD34+ cells to T Cells >
How correlative is the CFU assay to the engraftment efficiency of CD34+ cells in NSG mice?
Dr. Jackie Damen: There are a few examples of results from the CFU assays that correlate with good engraftment. Specifically, in a 2014 publication from Dr. Guy Sauvageau's lab (Fares et al, 2014), it was shown that when expanding cord blood CD34+ cells in the presence of UM171, there was an increase in the CD34+CD90+ population as well as in the numbers of the multipotential CFU-GEMM colonies. These two parameters correlated with an improvement in the frequency of HSCs, as determined by engraftment in the SCID repopulating cells (SRC) assay.
In addition, there seems to be good anecdotal data for this correlation: preliminary results presented in abstracts at meetings like ASH have shown trends in CFU frequency and colony size with engraftment potential and chimerism. Several translational studies have also concluded that the CFU-GM assay strongly correlates with successful patient recovery following a transplant.
We know also that when we expand CD34+ cells in culture, especially without the use of small molecules that support the self-renewing HSC divisions, and remove cells after 5 - 7 days to plate these in the CFU assay, two things are certain: the frequency of CFUs drop and colonies become smaller as their proliferative potential is exhausted. When there are no more progenitors that can be read out in the CFU assay, the expectation is that there would also be no cells capable of long term engraftment.
Further Reading
- Fares I et al. (2014) Pyrimidoindole derivatives are agonists of human hematopoietic stem cell self-renewal. Science (80) 345(6203): 1509–12.
Hematopoietic Colony Counting
Is trypan blue the most commonly used method for distinguishing live/dead, cells or would you recommend other stains? I noticed in your presentation that trypan staining-based cell counting can introduce errors from untrained personnel.
Dr. Jackie Damen: The use of trypan blue to evaluate cell viability has been used in cell culture for many years and can be performed manually (using a hemocytometer) or using automated cell counters. Viability determined manually with trypan blue is more subjective, based in part on the fact it is an exclusion dye compared to nuclear dyes like 7AAD that are more sensitive and robust. There is no consensus in the field to recommend a specific viability dye, but it is understood that trypan blue typically results in higher viability assessment when compared directly to 7AAD and AO/PI. Different viability stains can be used and validation with additional assays to confirm functional potency is typically required.
As far as a recommendation, I prefer using AO/PI staining. When we switched in the lab from using trypan blue to AO/PI, we realized that our viability for qualified lots of BM MNCs were in general ~10-15% lower but our CFU output was ~10 - 15% higher due to improved sensitivity of AO/PI compared to trypan blue.
How many cells do you use to seed one plate when establishing viability using the CFU Assay?
Dr. Jackie Damen: The seeding density is dependent on the cell source and species when plating in the CFU Assay. For human samples, this is dependent on the frequency of CD34+ expected in these samples. Since this can vary between donors, we recommend ranges and plating 2 - 3 cell concentrations within the ranges (provided in the webinar on slide 27 and listed below) to ensure the CFU frequency is within the linear range and detection limits of the CFU assay.
Alternatively, if the percentage of CD34+ cells is known, the expectation is that there would be ~25% CFU per CD34+ cell plated (Serke, S. et al., 1991). So a more specific and appropriate plating concentration can be calculated from the number of CD34+ for each sample before plating.
Further Reading
- Serke S et al. (1991) Analysis of CD34-positive hematopoietic progenitor cells from normal human adult peripheral blood: Flow-cytometrical studies and in-vitro colony (CFU-GM, BFU-E) assays. Ann Hematol 62(2–3): 45–53.
- Watts MJ & Linch DC. (2016) Optimisation and quality control of cell processing for autologous stem cell transplantation. Br J Haematol 175(5): 771–83.
Can you please expand on recombinant cytokines regarding CFU Assays?
Dr. Jackie Damen: Optimal combinations and cytokine concentrations have been the subject of many investigations and attempts to standardize the CFU assay over the last 30 years. For human CFUs, most media formulations require appropriately qualified FBS with cytokine combinations that are optimal for the growth and differentiation of each progenitor type.
To visualize all the potential progenitors in a single patient sample for myelopoiesis, cytokine combinations that support the simultaneous growth of erythroid and myeloid progenitors have included recombinant human cytokines for SCF, GM-CSF, EPO, G-CSF, IL-3 and, in some cases, IL-6 if CD34+ are first purified.
Is the scoring of CFU assays subjective?
Dr. Jackie Damen: Yes, the scoring of CFU assays can be subjective. Some of the most common and particularly challenging phenomena encountered when scoring CFU colonies is the presence of colonies with multiple foci or clusters, which can be scored as separate colonies and thus erroneously skew the total counts to higher CFU numbers. This, in turn, may lead to an overestimation of HSPC graft potency. Conversely, high plating concentrations can result in overlapping and underdeveloped colonies that can lead to under-scoring of CFUs. Training has been shown to improve consistency between manual counters with regard to both identification of colony number as well as lineage identification of each colony type.
Use STEMvision™ to increase accuracy of your colony counts >
How does STEMvision™ automated scoring compare to manual counting?
Dr. Jackie Damen: Validation studies to compare manual versus automated CFU counting have been investigated by various groups as part of their qualification process when switching from manual to automated CFU scoring. Internal studies carried out at STEMCELL show a strong correlation between manual and automated CFU scoring. These studies were carried out by comparing manual counts (performed by 3 to 7 experienced counters) of colony assays using cord blood, bone marrow, or mobilized peripheral blood, and comparing these counts to automated counts on a STEMvision™ instrument. Results showed an r value of 0.96 for total colonies, indicating a strong correlation between manual and automated CFU scoring.
More recently, Velier M et al. (2019) published that automated scoring using STEMvision™ reduces the coefficients of variation of repeatability, inter-operator variability, and intermediate precision.
Further Reading
- Velier M, et al. (2019) Validation of a semi automatic device to standardize quantification of colony-forming unit (CFU) on hematopoietic stem cell products. Cytotherapy 21(8): 820–23.
Can you give any examples on discrepancies between automated scoring and manual scoring?
Dr. Jackie Damen: When validating automated scoring, three errors can be identified: false positives (resulting from scratches or artifacts in the media and cultureware or overlapping colonies), false negatives (colonies not scored due to merging of colonies or colonies missed on the edges of the wells), and misidentified colonies (colonies that are scored as the wrong lineage).
Independent customer studies that have been shared with us have shown that correction of these errors, using the images available from colonies scored using STEMvision™ algorithms, resulted in data that was not statistically different. Differences in colony numbers and identification between corrected and uncorrected images were not significant. Similarly, the variability in counts from corrected and uncorrected images were shown to have similar or lower coefficients of variation (CVs) when using automated scoring compared to manual counting.
Find out more in the STEMvision™ Automated and Standardized Counting of CFU Assays for Cord Blood Banks Brochure.
Is there a way to use STEMvision™ algorithms with bifocal microscope-acquired images?
Dr. Jackie Damen: Imaging with STEMvision™ is key to the way the STEMvision™ algorithm works and the algorithm cannot be used seperately to score images of colonies taken with a digital camera as the entire image is required for scoring with the STEMvision™ algorithms.
Do you offer a ready-to-go cytokine mix as a supplement for the CFU assay?
Amanda Fentiman, MSc (Product Manager, Hematology): We offer complete media for CFU assays, MethoCult™, which consists of methylcellulose media and supplements with prequalified serum, and cytokines optimized for human or mouse hematopoietic colony growth. For human cells our MethoCult™ H4034 Optimum is the best media for myeloid and erythroid colony growth from blood or bone marrow. We also offer serum-free formulations and cytokine-free versions, depending on what you need.
Learn more about MethoCult™, the “Gold Standard” for the in vitro detection and quantification of hematopoietic progenitor cells >The regulations that we follow are from 1996, ISHAGE. Are there any actions by international societies when it comes to standardization of HCTPs?
Dr. Jackie Damen: There are other international societies, including the Joint Accreditation Committee ISCT-Europe (JACIE), which is an accreditation body for hematopoietic stem cell therapy. Their standards also require a potency assay for cell therapy products undergoing manipulation as well as for stability testing following storage. The CFU assay is suggested in addition to determination of CD34+ cell numbers; however, there is no mention of standardized protocols for these assays that I know of. Groups can validate their own assays and protocols and, with regards to those involving FACS, some publications have included the use of ALDH or the use of apoptotic dyes when evaluating viable CD34+ to ensure functional viability.
Questions have been condensed and edited for clarity.
Explore These Resources
Request Pricing
Thank you for your interest in this product. Please provide us with your contact information and your local representative will contact you with a customized quote. Where appropriate, they can also assist you with a(n):
Estimated delivery time for your area
Product sample or exclusive offer
In-lab demonstration